Hiring and job searching are difficult in many industries, but among the most challenging is healthcare.
Healthcare jobs are specialized, and they generally tend to be highly competitive to get. Plus, salaries aren’t always listed, and some jobs posted may be fake. What’s more, most healthcare professionals are already working demanding roles so their time to search for a new job is limited.
Sheldon Arora saw a need — and the potential — for a better way to connect healthcare job seekers with employers.
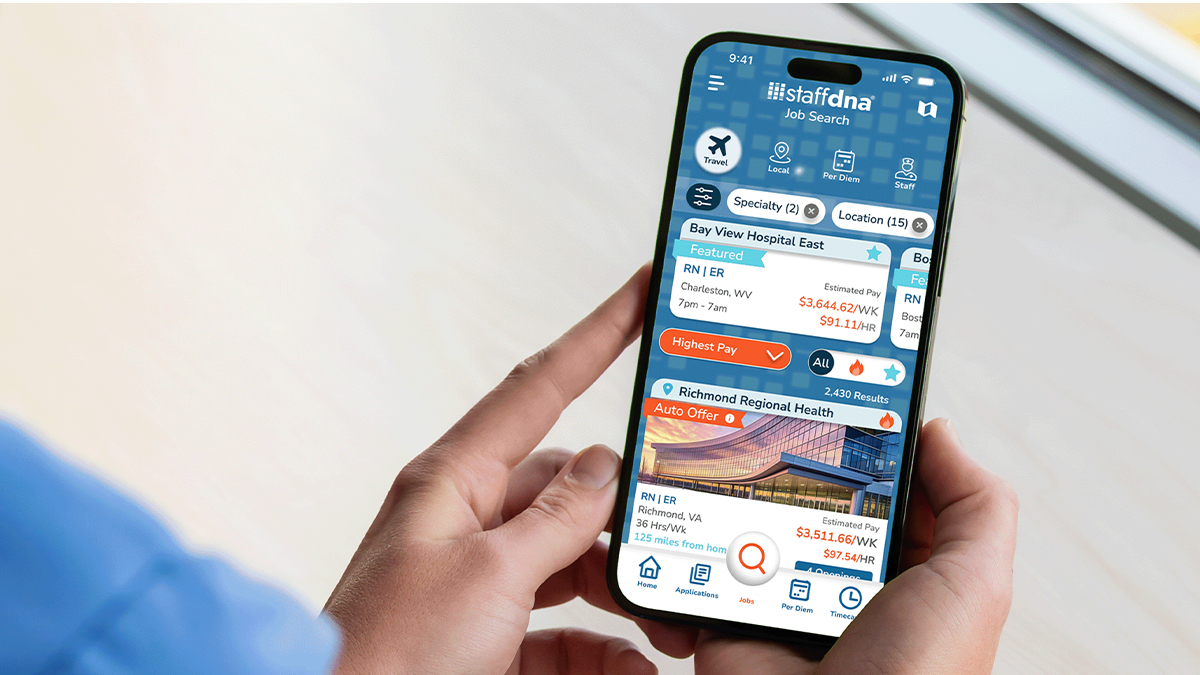
That’s why Arora designed StaffDNAⓇ, a mobile app that helps facilitate filling healthcare roles, benefitting employers and job seekers alike.
StaffDNA is available to download for free on the Apple Store and Google Play.
Meeting a need

Sheldon Arora
Founder and CEO, StaffDNA
Arora, the CEO of StaffDNA, realized early in his career that hiring was an inefficient process. As a tech entrepreneur, he started companies that helped solve the most challenging aspects of matching employees with the right role at the right time. The industry he noticed had the most inefficient hiring process and could benefit the most from the right technology was healthcare.
“We were looking for ways to make the hiring process in healthcare more efficient for a long time,” Arora said. “We saw that facilities needed on-demand access to healthcare professionals, and healthcare professionals needed more options and transparency in their job searches.”
The resource combines a self-service app with a search platform for various needs for healthcare in all professions, specialties, job types, and settings.
“We built a platform where job seekers and facility hiring managers could connect in real time, and we removed many layers and obstacles that stood in the way of connecting people looking to find the jobs they loved. We knew we wanted to improve the entire process, so we did just that,” said Arora, who launched the app about one month before the start of the COVID-19 pandemic, when healthcare jobs were needed most. Downloads skyrocketed.
How it works
“The StaffDNA marketplace is the only platform where all stakeholders in the hiring process, including hospitals, vendors, suppliers, and job seekers, can come together to address the healthcare staffing issue once and for all,” said Arora, adding that candidates can search, apply, and get hired all within the StaffDNA app. “We’re tying together all the participants in healthcare hiring and giving them the platform they need to efficiently get people hired in the right roles.”
In the StaffDNA app, all jobs, specialties, and locations, as well as job descriptions and compensation, are shown up front. “Everything they need can be found directly in the app, from employment in their area to facility details, and even the color of scrubs they’ll need to wear,” Arora noted. “We also give candidates the ability to customize pay packages based on housing and benefit needs so they can have a better idea of what their take-home pay will be.”
Helpful features
Two new features of the StaffDNA app — DNAVault™ and DNAInsights™ — make the app even more beneficial for job seekers and hiring professionals.
DNAVault allows anyone — job seekers, students, or professionals in any industry — to securely store sensitive documents, including licenses and credentials. The app makes it easy and convenient to keep these materials safely in one place, and applicants can send these items directly to their employer, school, or anyone through DNAVault’s secure online storage. DNAVault will also notify users when their documents are about to expire so they know when to renew them.
“The inspiration for DNAVault came from my daughter, Madison, who is in medical school,” Arora said. “She was explaining how many documents and certifications she needed to keep track of and how they were required to access them from anywhere.”
DNAInsights was created for healthcare facilities. It offers data on the number of job openings within a given radius, along with competitive pay rates, which are critical resources for hospital hiring managers. StaffDNA is the first company to provide healthcare facilities with real-time job data for all per-diem, travel, local, and staff positions — for free. “Until now, hiring managers in healthcare have had no tools to gauge pay rates in their markets,” Arora said. “So, we built the technology to support how hospitals and facilities determine pay rates when hiring.”
Making a difference
StaffDNA has been downloaded 2 million times and counting, and Arora has heard from users about its real-life impacts, including candidates taking dream vacations due to high-paying assignments or exploring the country through travel assignments they’ve picked up through the app.
Arora shared that he was attending a healthcare industry conference in Las Vegas when a nurse told him she got a pay raise thanks to StaffDNA. “She said she was working at a hospital and saw a job opening in her profession, which paid more than what she was currently earning,” he said. “She used the data to request an hourly pay raise, and she got it. She thanked me for helping her earn a better income. It was exciting to hear her story.”
Arora is hopeful the app has a broader impact, too — that is, not only on the people using the app but public health as a whole.
“Through StaffDNA, healthcare professionals are empowered to find jobs they love, and hiring facilities can hire the right people for the right roles,” Arora said. “When these two things come together, we know ultimately patient care is improved and communities thrive.”
Click here to download the StaffDNA app